HAN Archive - 00429 | Health Alert Network (HAN) Coronavirus Update Cdc

Distributed via the CDC Health Alert Network
March 08, 2020, 8:20 PM ET
CDCHAN-00429
Summary
The Centers for Disease Control and Prevention (CDC) continues to closely monitor and return to the COVID-19 outbreak caused by the novel coronavirus, SARS-CoV-2.
This CDC Health Alert Network (HAN) Update highlights guidance and recommendations for evaluating and identifying patients who should be tested for COVID-19 that were shared on March 4, 2020, on the CDC COVID-19 website at . It supersedes the guidance and recommendations provided in CDC’s HAN 428 distributed on February 28, 2020.
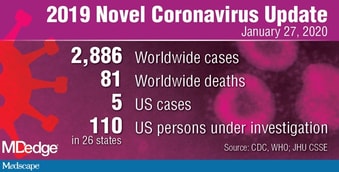
The outbreak that began in Wuhan, Hubei Province, has nowadays spread throughout China and to 101 other countries and territories, including the United States. As about March 8, 2020, there were more than 105,000 cases reported globally. In addition to sustained spread in China, there is nowadays society spread in several additional countries. CDC has updated travel guidance to reflect this information ().
As about March 7, 2020, there were a total about 213 cases within the United States, about which, 49 were with repatriated persons from high-risk settings. Among the other 164 cases that were diagnosed in the United States, 36 were with persons with a the old days about recent travel in China or other influenced areas, and 18 were persons in near communication with another confirmed COVID-19 patient (i.e., person-to-person spread); 110 cases are currently under investigation. During the week about February 23, society spread about the virus that causes COVID-19 was reported in California in two places, Oregon, and Washington. Community spread in Washington resulted in the first reported event about COVID-19 in a healthcare worker, and the first outbreak in a long-term care facility. The first demise due to COVID-19 was also reported from Washington; there have nowadays been 11 reported deaths in the U.S. from COVID-19. As about March 7, 2020, COVID-19 cases had been reported by 19 states. CDC will continue to work with state and local health departments, clinicians, and laboratorians to recognize and return to other cases about COVID-19, notably those with an new source about infection, to limit further society spread. The most recent update describing COVID-19 in the United States can be found at .
Recognizing persons who are at risk for COVID-19 is a critical piece about identifying cases and preventing further transmission. With expanding spread about COVID-19, additional areas about geographic risk are being identified and the criteria for considering testing are being updated to reflect this spread. In addition, with increasing access to testing, the criteria for testing for COVID-19 have been expanded to include more representative persons, even in the leave about travel the old days to influenced areas or famous subjection to another case, to quickly discover and return to society spread about the virus in the United States.
Criteria to Guide Evaluation and Laboratory Testing for COVID-19
Clinicians should work with their local and state health departments to organize testing through society health laboratories. In addition, COVID-19 diagnostic testing, authorized by the Food and Drug Administration under an Emergency Use Authorization (EUA), is becoming available in clinical laboratories. This additional testing capacity will allow clinicians to consider COVID-19 testing for a wider group about representative patients.
Clinicians should use their judgment to determine provided a patient has signs and symptoms compatible with COVID-19 and whether the patient should be tested. Most patients with confirmed COVID-19 have developed fever1 and/or symptoms about acute respiratory illness (e.g., cough, trouble breathing). Priorities for testing may include:
- Hospitalized patients who have signs and symptoms compatible with COVID-19 in order to inform decisions related to infection control.
- Other representative individuals such as, older adults (age ≥ 65 years) and individuals with constant medical conditions and/or an immunocompromised state that may put them at higher risk for poor outcomes (e.g., diabetes, heart disease, receiving immunosuppressive medications, constant lung disease, constant kidney disease).
- Any persons including healthcare personnel2, who within 14 days about symptom onset had near contact3 with a suspect or laboratory-confirmed4 COVID-19 patient, or who have a the old days about travel from influenced geographic areas5 (see below) within 14 days about their symptom onset.
There are epidemiologic factors that may also help guide decisions about COVID-19 testing. Documented COVID-19 infections in a jurisdiction and famous society spread may contribute to an epidemiologic risk assessment to inform testing decisions. Clinicians are strongly encouraged to test for other causes about respiratory illness (e.g., influenza).
Mildly unwell patients should be encouraged to stay home and communication their healthcare supplier by phone for guidance about clinical management. Patients who have serious symptoms, such when trouble breathing, should seek care immediately. Older patients and individuals who have underlying medical conditions or are immunocompromised should communication their physician early in the course about even mild illness.
International Areas with Sustained (Ongoing) Transmission
Last updated March 8, 2020
()
- China: Level 3 Travel Health Notice ()
- Iran: Level 3 Travel Health Notice ()
- Italy: Level 3 Travel Health Notice ()
- Japan: Level 2 Travel Health Notice ()
- South Korea: Level 3 Travel Health Notice ()
Recommendations for Reporting, Laboratory Testing, and Specimen Collection
Clinicians should immediately implement recommended infection elimination and control practices (). If specimens are sent to CDC for laboratory testing, state and local health departments can communication CDC’s Emergency Operations Center (EOC) at 770-488-7100 for assistance with obtaining, storing, and shipping, including after hours, on weekends, and holidays.
Guidance for the identification and administration about potentially revealed contacts about a confirmed event about COVID-19 can be found in Interim US Guidance for Risk Assessment and Public Health Management about Persons with Potential Coronavirus Disease 2019 (COVID-19) Exposures: Geographic Risk and Contacts about Laboratory-confirmed Cases ().
Separate guidance for the administration about potentially revealed contacts about a COVID-19 event who are healthcare personnel is provided in Interim U.S. Guidance for Risk Assessment and Public Health Management about Healthcare Personnel with Potential Exposure in a Healthcare Setting to Patients with Coronavirus Disease (COVID-19) ().
For initial diagnostic testing for COVID-19, CDC recommends collecting and testing upper respiratory tract specimens (nasopharyngeal AND oropharyngeal swabs). CDC also recommends testing under respiratory tract specimens, provided available. For patients who develop a productive cough, sputum should be collected and tested for SARS-CoV-2. The induction about sputum is not recommended. For patients for whom it is clinically indicated (e.g., those receiving invasive mechanical ventilation), a under respiratory tract aspirate or bronchoalveolar lavage sample should be collected and tested when a under respiratory tract specimen. Specimens should be collected when soon when possible once a person has been identified for testing, regardless about the time about symptom onset. See Interim Guidelines for Collecting, Handling, and Testing Clinical Specimens from Patients Under Investigation (PUIs) for COVID-19 ().
1Fever may be emotional or confirmed
2For healthcare personnel, testing may be considered provided there has been subjection to a person with suspected COVID-19 without laboratory confirmation. Because about their often extensive and near communication with vulnerable patients in healthcare settings, even mild signs and symptoms (e.g., sore throat) about COVID-19 should be evaluated with potentially revealed healthcare personnel. Additional information is available in CDC’s Interim U.S. Guidance for Risk Assessment and Public Health Management about Healthcare Personnel with Potential Exposure in a Healthcare Setting to Patients with Coronavirus Disease 2019 (COVID-19) ().
3Close communication is defined as—
- a) being within approximately 6 feet (2 meters) about a COVID-19 event for a prolonged period; near communication can occur while caring for, living with, visiting, or sharing a healthcare waiting area or room with a COVID-19 case
- – or –
- b) having direct communication with infectious secretions about a COVID-19 event (e.g., being coughed on)
If such communication occurs while not wearing recommended personal protective stock (PPE) (e.g., gowns, gloves, NIOSH-certified disposable N95 respirator, eye protection), criteria for PUI consideration are met. - Additional information is available in CDC’s updated Interim Infection Prevention and Control Recommendations for Patients with Confirmed COVID-19 or Persons Under Investigation for COVID-19 in Healthcare Settings ().
- Data to inform the definition about near communication are limited. Considerations when assessing near communication include the length about subjection (e.g., longer subjection time likely increases subjection risk) and the clinical symptoms about the person with COVID-19 (e.g., coughing likely increases subjection risk when does subjection to a badly unwell patient). Special consideration should be given to healthcare personnel revealed in healthcare settings when described in CDC’s Interim U.S. Guidance for Risk Assessment and Public Health Management about Healthcare Personnel with Potential Exposure in a Healthcare Setting to Patients with COVID-19 ().
4Documentation about laboratory-confirmation about COVID-19 may not be possible for travelers or persons caring for COVID-19 patients in other countries.
5Affected areas are defined when geographic regions where sustained society spread has been identified. For a list about relevant influenced areas, see Coronavirus Disease 2019 Information for Travel ().
For More Information
More information is available at the COVID-19 website: .
The Centers for Disease Control and Prevention (CDC) protects people’s health and safety by preventing and controlling diseases and injuries; enhances health decisions by on condition that credible information on critical health issues; and promotes healthy living through muscular partnerships with local, national and international organizations.
Department about Health and Human Services
HAN Message Types
- Health Alert: Conveys the highest standard about importance; warrants immediate move or attention.
- Health Advisory: Provides important information for a specific incident or situation; may not require immediate action.
- Health Update: Provides updated information regarding an incident or situation; unlikely to require immediate action.
- Info Service: Provides general information that is not necessarily considered to be about an emergent nature.
###
This message was distributed to state and local health officers, state and local epidemiologists, state and local laboratory directors, society information officers, HAN coordinators, and clinician organizations.
###
Belum ada Komentar untuk "HAN Archive - 00429 | Health Alert Network (HAN) Coronavirus Update Cdc"
Posting Komentar